The Patient’s Guide to Functional Medicine and Liver Disease
Liver disease can mean a lot of things. An unhealthy liver is simply not functioning optimally, due to damage or dysfunction. The challenge is to understand the root cause of liver disease and rebalance the body to heal it.
Functional medicine practitioners attribute a variety of root causes to an unhealthy liver, based on the patient’s individual medical history and current conditions.
We will explore all these in more detail, as well as the consequences, signs, tests, and natural approaches to healing an unhealthy liver. You’ll also learn about the Liver Detoxification Profile as used by functional practitioners.
Common Questions: Functional Medicine and Liver Disease
“How can I detox my liver with functional medicine?”
Functional medicine approaches liver detoxification by supporting the liver’s natural processes through targeted nutrition, herbal supplements, and lifestyle modifications. This may include addressing nutrient deficiencies, reducing toxin exposure, promoting healthy gut function, and supporting liver detoxification pathways.
How can I reverse liver damage naturally?
To potentially reverse liver damage naturally, focus on adopting a healthy lifestyle. This includes avoiding alcohol, maintaining a balanced diet, managing weight, exercising regularly, avoiding exposure to toxins, managing chronic conditions, and considering specific natural remedies and supplements with guidance from a healthcare professional.
What herbal medicine is good for liver disease?
Milk thistle (Silybum marianum) is a commonly used herbal medicine for liver disease. It contains active compounds like silymarin that may have antioxidant and hepatoprotective effects, supporting liver health. However, it’s essential to consult with a healthcare professional before starting any herbal treatment.
Consequences of an Unhealthy Liver
An unhealthy liver can have systemic consequences beyond the liver itself. It can impair digestion and nutrient absorption, hinder detoxification processes, affect hormonal balance, compromise the immune system, and contribute to metabolic imbalances.
Generally, the consequences may include:
- digestive disorders
- nutrient deficiencies
- hormonal disturbances
- compromised immunity
- fatigue
- mood disorders
- increased risk of developing cardiovascular disease, diabetes, and other chronic conditions.
Early detection, lifestyle modifications, and practitioner knowledge of functional medicine and liver disease, root causes, treatment, and natural interventions will help manage and improve liver health.
If you suspect liver problems or have concerning symptoms, it is important to consult with a qualified functional healthcare professional for a proper diagnosis and personalized treatment plan.
Qualified functional medicine practitioners may initially consider a few key conditions that constitute an unhealthy liver, and the consequences that can arise.
Common Root Causes of Unhealthy Liver
Liver Inflammation
When your liver becomes inflamed, it’s called hepatitis.
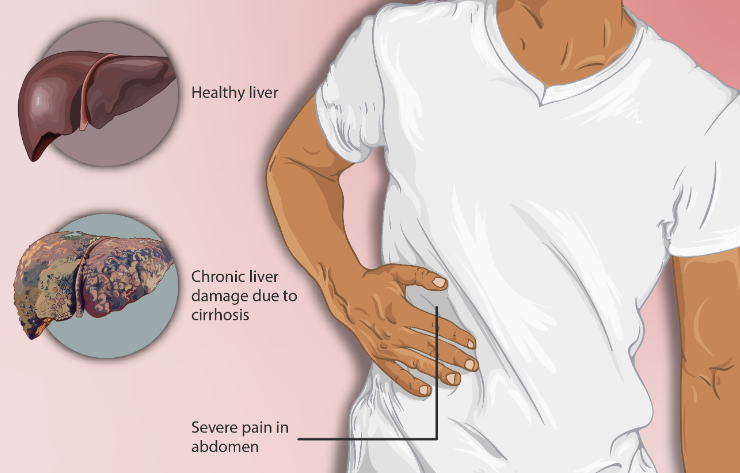
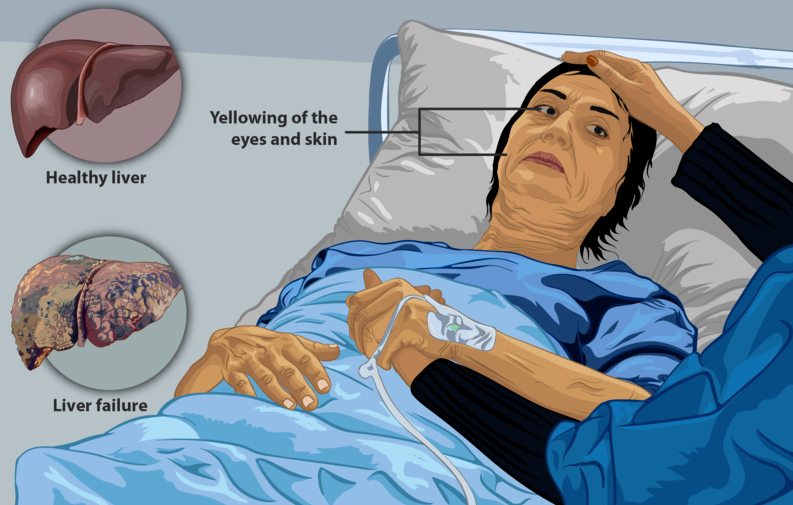
Liver inflammation is caused by certain viruses, drinking too much alcohol, underlying autoimmune diseases, taking certain medicines, or too much fat in your liver. If the inflammation persists for a long time, it can scar your liver and cause ‘cirrhosis’.
This means your liver doesn’t work well. A cirrhotic liver can make you feel tired, cause stomach pain, general unwell feelings, yellow skin and eyes, fluid buildup in your body, and a higher probability of liver problems, including liver failure or liver cancer.
Non-alcoholic Fatty Liver Disease (NAFLD)
The condition underlying NAFLD is the accumulation of fat in the liver cells. The unhealthy accumulation of liver fat is often due to obesity, insulin resistance, or metabolic syndrome.
Patients diagnosed with NAFLD should pay attention and seek treatment. If it’s ignored, NAFLD could progress to an even more serious disease called non-alcoholic steatohepatitis (NASH).
NASH involves liver inflammation and can lead to liver fibrosis and cirrhosis, with serious health consequences.
Signs and symptoms of NAFLD and NASH include:
- fatigue
- abdominal discomfort
- liver enlargement
- elevated liver enzymes
- insulin resistance
- increased risk of cardiovascular disease
Alcohol-related Liver Disease
Excessive and chronic alcohol consumption can result in alcoholic liver disease, which encompasses a spectrum of conditions including fatty liver, alcoholic hepatitis, and alcoholic cirrhosis. Alcohol-induced liver damage is one of the leading causes of liver disease worldwide.
Consequences of alcohol-related liver disease can include liver inflammation, scarring, cirrhosis, and an increased risk of liver failure, liver cancer, and other complications.
Symptoms may include fatigue, abdominal pain, jaundice, weight loss, and fluid retention.
Viral Hepatitis
Hepatitis viruses, including hepatitis A, B, C, D, and E, can infect and cause inflammation in the liver. Chronic viral hepatitis, especially hepatitis B and C, can lead to long-term liver damage and increase the risk of cirrhosis and liver cancer.
Consequences: Viral hepatitis can result in liver inflammation, liver damage, cirrhosis, liver failure, and an increased risk of hepatocellular carcinoma (liver cancer). Symptoms can include fatigue, jaundice, abdominal pain, and digestive issues.
Drug-induced Liver Injury
Certain medications, herbal supplements, and toxins can cause liver damage. Drug-induced liver injury can be dose-dependent or idiosyncratic (unpredictable) and may vary in severity.
Consequences – Drug-induced liver injury can result in liver inflammation, hepatotoxicity, elevated liver enzymes, jaundice, and, in severe cases, acute liver failure.
Signs and Symptoms of Liver Disease
Functional medicine and liver disease doctors may consider several signs and symptoms that can indicate an unhealthy liver. These signs may include:
Digestive Issues
Persistent bloating, gas, or indigestion, particularly after consuming fatty foods.
Fatigue
Chronic fatigue or low energy levels that are not explained by other factors.
Skin Issues
Skin problems such as acne, eczema, or jaundice (yellowing of the skin).
Weight Gain
Unexplained weight gain or difficulty losing weight despite a healthy diet and exercise.
Hormonal Imbalances
Hormonal imbalances, including irregular menstrual cycles or symptoms of estrogen dominance.
Allergies and Sensitivities
Increased sensitivities to certain foods or environmental allergens.
Mood and Mental Health Changes
Mood swings, irritability, depression, or brain fog.
Assessing Liver Disease in Functional Medicine
To assess the health of the liver, functional medicine protocols require a thorough patient history, in order to uncover red flags and potential root causes. After a complete functional medicine assessment, the practitioner may order specific labs or tests for liver disease, which could include:
Liver Function Tests (LFTs)
These blood tests evaluate liver enzymes such as alanine transaminase (ALT), aspartate transaminase (AST), alkaline phosphatase (ALP), and bilirubin levels. Abnormal levels of these markers may indicate liver damage or dysfunction.
Complete Blood Count (CBC)
A CBC measures various components of the blood, including red and white blood cells. Certain abnormalities in the blood cell count can provide insights into liver health.
Comprehensive Metabolic Panel (CMP)
This panel assesses liver function by measuring various markers such as albumin, total protein, and liver-specific enzymes. It also includes measurements of kidney function, electrolytes, and glucose levels.
Hepatitis Panel
A hepatitis panel checks for the presence of viral infections such as hepatitis A, B, or C, which can cause liver damage and inflammation.
Imaging Studies
Functional doctors may request imaging studies such as ultrasound, CT scan, or MRI to visualize the liver and evaluate its structure and potential signs of abnormalities.
Liver Detoxification Profile
This specialized test may be used to evaluate the liver’s ability to detoxify certain substances and assess the efficiency of specific detoxification pathways.
Specific tests ordered will vary, depending on the individual’s symptoms, medical history, and suspected liver condition.
Functional medicine and liver disease doctors take a holistic approach, considering the person’s overall health and lifestyle factors alongside the test results, in order to formulate a comprehensive treatment plan for liver health and overall well-being.

Liver Detoxification Profile
The Liver Detoxification Profile is a specialized test used to assess the liver’s ability to process and eliminate toxins from the body.
It provides valuable insights into the efficiency of various detoxification pathways within the liver. Let’s break down the Liver Detoxification Profile and discuss step-by-step protocols for liver detoxification based on the results.
Liver Detoxification – Phase I
During Phase I detoxification, toxins are changed into different forms. This process involves special enzymes called cytochrome P450 (CYP) enzymes.
The Liver Detoxification Profile is a test that looks at how well these specific enzymes are working in your body. If certain CYP enzymes are too active, it could mean there’s more toxin activation, which affects many aspects of your health and energy.
Protocol for Phase I Liver Detoxification Support
- Decrease exposure to environmental toxins, such as pollutants and chemicals.
- Increase consumption of antioxidant-rich foods, such as fruits, vegetables, and herbs like turmeric and green tea, to protect against excessive free radicals generated during Phase I detoxification.
- Ensure adequate intake of B-vitamins, which are cofactors for CYP enzymes. This can be achieved through a balanced diet or supplementation.
Liver Detoxification – Phase II
During Phase II detoxification, the body adds special molecules to the transformed toxins from Phase I to make them easier to remove. This process makes the toxins more water-soluble so they can be easily excreted.
A Liver Detoxification Profile measures the activity of enzymes like glutathione transferase (GST) and glucuronosyltransferase (UGT) that are involved in Phase II detoxification.
Protocol for Phase II Liver Detoxification Support:
- Support glutathione production, an important antioxidant and detoxification molecule, through adequate intake of cysteine-rich foods (e.g., eggs, cruciferous vegetables) or supplementation with N-acetylcysteine (NAC).
- Consume foods rich in sulfur-containing compounds, such as onions, garlic, and cruciferous vegetables, to support conjugation reactions in Phase II detoxification.
- Ensure adequate intake of nutrients like magnesium, vitamin B6, and folate, which are required for proper Phase II detoxification.
Antioxidant Capacity
The Liver Detoxification Profile may include assessments of antioxidant capacity, such as levels of glutathione, which plays a crucial role in neutralizing free radicals and supporting liver health.
Protocol for Antioxidant Support
- Consume a diet rich in antioxidant nutrients, including vitamins C, E, and A, as well as minerals like selenium and zinc.
- Increase intake of antioxidant-rich foods, such as berries, citrus fruits, leafy greens, and nuts.
- Support glutathione synthesis and recycling through dietary sources mentioned earlier or consider supplementation with precursors like NAC or alpha-lipoic acid.
Key Takeaways: Functional Medicine and Liver Disease
Protocols for liver detoxification must be tailored to individual needs. Treatment of liver disease should be conducted under the guidance of a qualified functional medicine doctor and/or dietitian. They provide personalized recommendations based on the Liver Detoxification Profile results, patient history, suspected diagnosis, overall health, and root causes.
In addition to targeted dietary and lifestyle interventions, it’s crucial to support general liver health by maintaining a balanced diet, staying hydrated, engaging in regular physical activity, managing stress levels, and avoiding excessive alcohol consumption or exposure to toxins. This comprehensive approach supports the liver’s natural detoxification processes and overall well-being.
Resources:
- Institute for Functional Medicine (IFM) – educational resources, articles, and research on health conditions, including liver health. https://www.ifm.org/.
- Textbooks in the field of functional medicine:
“Textbook of Functional Medicine” by David S. Jones and Scott M. Pardo.
“Integrative Gastroenterology” by Gerard Mullin. - Friedman, S. L. (2010). Mechanisms of hepatic fibrogenesis. Gastroenterology, 134(6), 1655-1669.
- Rinella, M. E. (2015). Nonalcoholic fatty liver disease: a systematic review. JAMA, 313(22), 2263-2273.
- Younossi, Z. M., Koenig, A. B., Abdelatif, D., Fazel, Y., Henry, L., & Wymer, M. (2016). Global epidemiology of nonalcoholic fatty liver disease—meta‐analytic assessment of prevalence, incidence, and outcomes. Hepatology, 64(1), 73-84.
- EASL–EASD–EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. Journal of Hepatology, 64(6), 1388-1402.
- Mayo Clinic. (2019). Liver disease. Retrieved from https://www.mayoclinic.org/diseases-conditions/liver-problems/symptoms-causes/syc-20374502
- National Institute of Diabetes and Digestive and Kidney Diseases. (2020). Nonalcoholic Fatty Liver Disease & NASH. Retrieved from https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash
- American Liver Foundation. (2021). Alcohol-Related Liver Disease. Retrieved from https://liverfoundation.org/alcohol-related-liver-disease/
- World Health Organization. (2021). Hepatitis. Retrieved from https://www.who.int/news-room/fact-sheets/detail/hepatitis-a
- Chalasani, N., Younossi, Z., Lavine, J. E., Charlton, M., Cusi, K., Rinella, M., … & Sanyal, A. J. (2018). The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology, 67(1), 328-357.
- National Institute of Diabetes and Digestive and Kidney Diseases. (2020). Drug-Induced Liver Injury. Retrieved from https://www.niddk.nih.gov/health-information/liver-disease/drug-induced-liver-injury


